Have you ever glanced at your hands or legs and noticed your veins standing out more than usual—almost as if they appeared overnight? For many people, this might seem like a harmless curiosity. But for others, it raises an important question: are these visible veins a normal sign of health, a part of aging, or could they be a sign of something more concerning happening beneath the skin? While visible veins are often dismissed as a simple cosmetic issue, health professionals caution that in some cases, they may indicate underlying circulation problems that deserve closer attention. Understanding why veins become more visible—and when to take it seriously—can help you make informed decisions about your health and peace of mind.
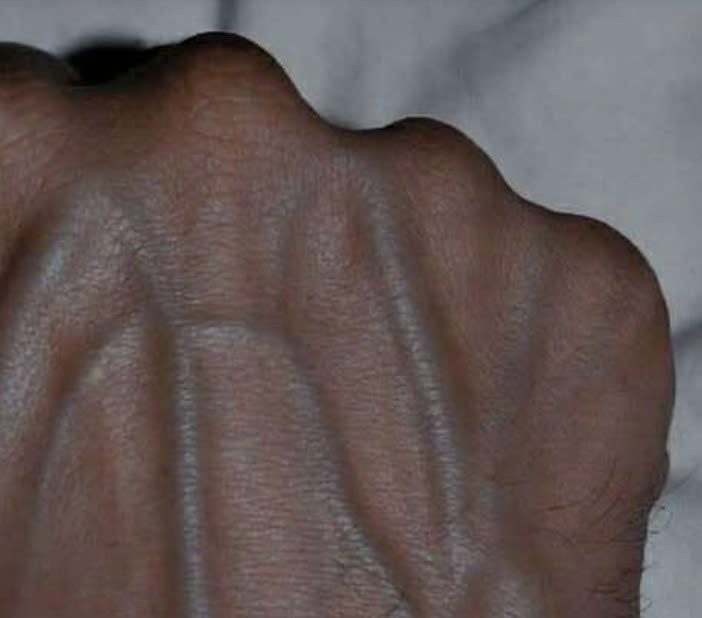
Veins play an essential role in your circulatory system, carrying oxygen-depleted blood back to the heart. Unlike arteries, veins sit closer to the surface of the skin and are more easily affected by both internal and external factors such as temperature, body fat, and even lifestyle choices. Several common, harmless reasons explain why your veins may become more noticeable. One of the most common causes is low body fat. When there’s less fat between your skin and veins, it’s natural for them to be more visible, especially in athletes, bodybuilders, or individuals who have lost weight quickly. Another major factor is aging. As people get older, their skin becomes thinner and less elastic, allowing veins to show through more clearly. Exercise and overall fitness can also make veins stand out, as physical activity increases blood flow, causing veins to expand. For those who are particularly active, this effect might persist even after the workout.
Warm weather can also play a role. When temperatures rise, veins expand to help cool the body, making them easier to see. Genetics is another key factor—if your parents or grandparents had visible veins, there’s a good chance you may develop them too, regardless of your overall health. In all these cases, visible veins are generally nothing to worry about and reflect natural, physical, or lifestyle-related changes.
However, sometimes visible veins can point to something more serious. If veins suddenly become more prominent without clear reason or if they’re accompanied by other symptoms like swelling, pain, or skin discoloration, it could signal an underlying medical condition. One such condition is chronic venous insufficiency (CVI), which happens when the valves in your veins weaken or fail to function properly. This can cause blood to pool in the legs, leading to swelling, heaviness, and bulging veins. Another related issue is varicose veins, which are enlarged, twisted veins often associated with aching, itching, or darkened skin.
Superficial thrombophlebitis is another condition to be aware of—it occurs when a small blood clot forms in a vein near the skin’s surface, causing redness, tenderness, and a firm, rope-like feeling along the vein. While it may sound alarming, it usually resolves with medical care. More concerning, however, is deep vein thrombosis (DVT), a serious and potentially life-threatening condition where a blood clot forms in a deep vein, usually in the leg. Symptoms include sudden swelling, warmth, redness, and pain in the affected area. DVT requires immediate medical attention because clots can travel to the lungs and cause a pulmonary embolism.
In addition to these medical causes, there are also temporary triggers that can make your veins appear more visible without indicating a serious problem. For instance, intense workouts or heavy weight training can cause veins to enlarge temporarily due to increased blood flow. Dehydration can also make veins stand out because lower fluid levels in the body cause veins to become more pronounced. Hormonal changes related to pregnancy, menstruation, or menopause can influence vein visibility as well. Rapid or sudden weight loss may also lead to more visible veins since the layer of fat under the skin becomes thinner.
So, when should you seek medical advice? If your veins suddenly become more visible without an obvious reason, or if you notice discomfort, pain, swelling, or changes in skin texture or color around them, it’s best to consult a healthcare professional. These symptoms can sometimes indicate circulation issues that require treatment. A doctor can help determine whether your visible veins are harmless or part of a larger vascular condition.
When it comes to treatment and management, there are several approaches depending on whether your concern is cosmetic or medical. Lifestyle changes are often the first line of defense—maintaining a healthy weight, staying active, elevating your legs when resting, and avoiding long periods of sitting or standing can all help. Wearing compression stockings can improve blood circulation and reduce swelling, especially for those who spend much of their day on their feet. For more persistent or severe cases, medical treatments like sclerotherapy (injections that close small veins), laser therapy, or minor surgical procedures may be recommended by your doctor.
Prevention is just as important as treatment. Staying hydrated, moving regularly—especially on long trips or during desk work—avoiding smoking, and eating a balanced, nutrient-rich diet all contribute to healthy circulation. Simple habits like stretching your legs, walking during breaks, or gently massaging your calves can also make a difference in how your veins look and feel over time.
Beyond health concerns, it’s worth noting the emotional and aesthetic side of visible veins. For athletes and fitness enthusiasts, pronounced veins are often seen as a sign of strength, conditioning, and dedication. For others, they may trigger self-consciousness or discomfort, especially when they appear suddenly or become more pronounced with age. The good news is that whether your concern is physical or cosmetic, there are solutions available to address both the health and appearance of your veins.
In the end, visible veins are usually nothing to fear. In most cases, they’re a natural result of genetics, aging, or lifestyle habits. But sometimes, they can reveal deeper circulatory issues such as venous insufficiency or blood clots that need professional care. The key is learning to recognize the difference between normal changes and potential warning signs. Paying attention to your body and consulting your doctor when something feels off can make all the difference. Your veins do more than carry blood—they offer important clues about your body’s overall circulatory health and well-being. So, the next time you notice your veins becoming more visible, take a moment to listen to what your body might be trying to tell you. And if in doubt, always seek expert advice. Sharing this information with family and friends could help someone else understand their own health a little better too.